Posted by Behavioral Health Billing Solutions, LLC.

The Bi-weekly meeting of the Medicaid EDI work-group was held yesterday down at Ohio Medicaid. A few important things to note:
1. Ohio BH Redesign go live is currently on hold. This doesn’t mean it’s cancelled, however, what delay is achieved will depend on the JCARR meeting on June 19th and the Ohio Senate vote on the budget next week which includes a 6 month delay to both the BH Redesign and the go-live for Managed Care.
2. We still have a HIGH amount of BH Medicaid Provider types 84 and 95 that do not have affiliated providers. Some may be due to inactive numbers listed, however, when it was originally pulled by Medicaid, they pulled Medicaid Providers with billing activity in 2016. Registering and Affiliating providers to your agency Medicaid number is a required FIRST step in the Redesign. Medicaid has started an automated call program to reach out to the remaining providers. Without affiliated providers, you may not be able to bill but you ABSOLUTELY will not be able to request a prior authorization which is required for some services.
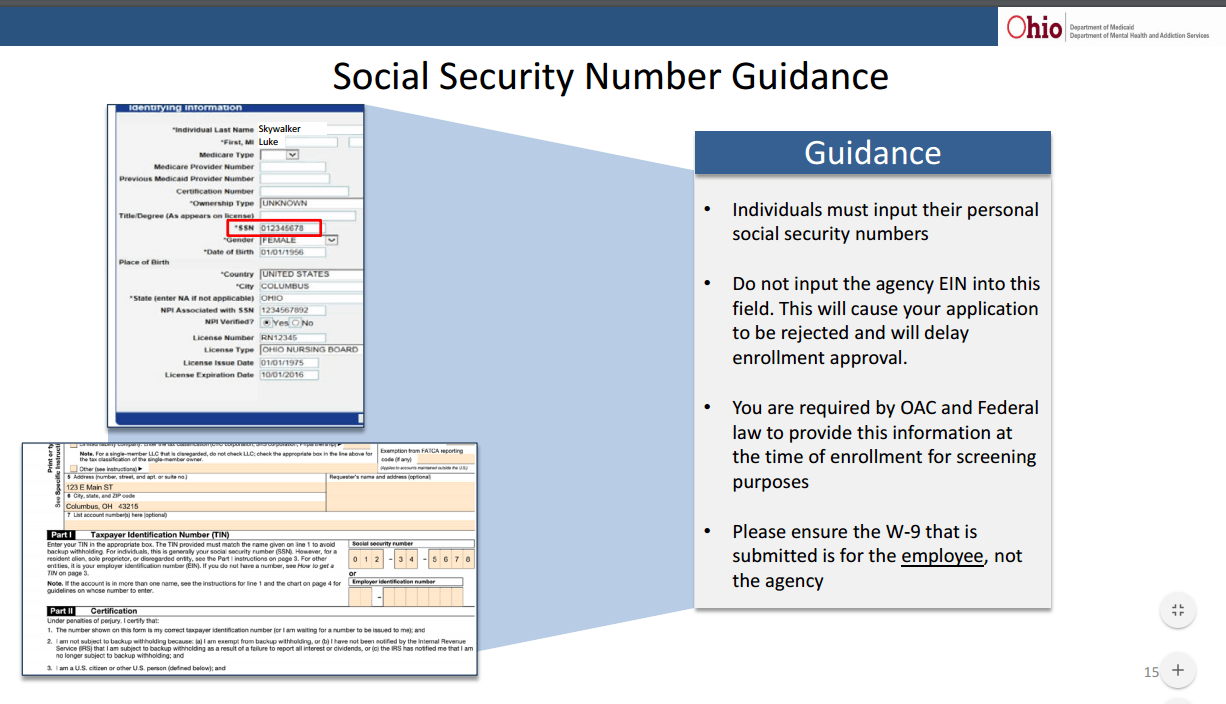
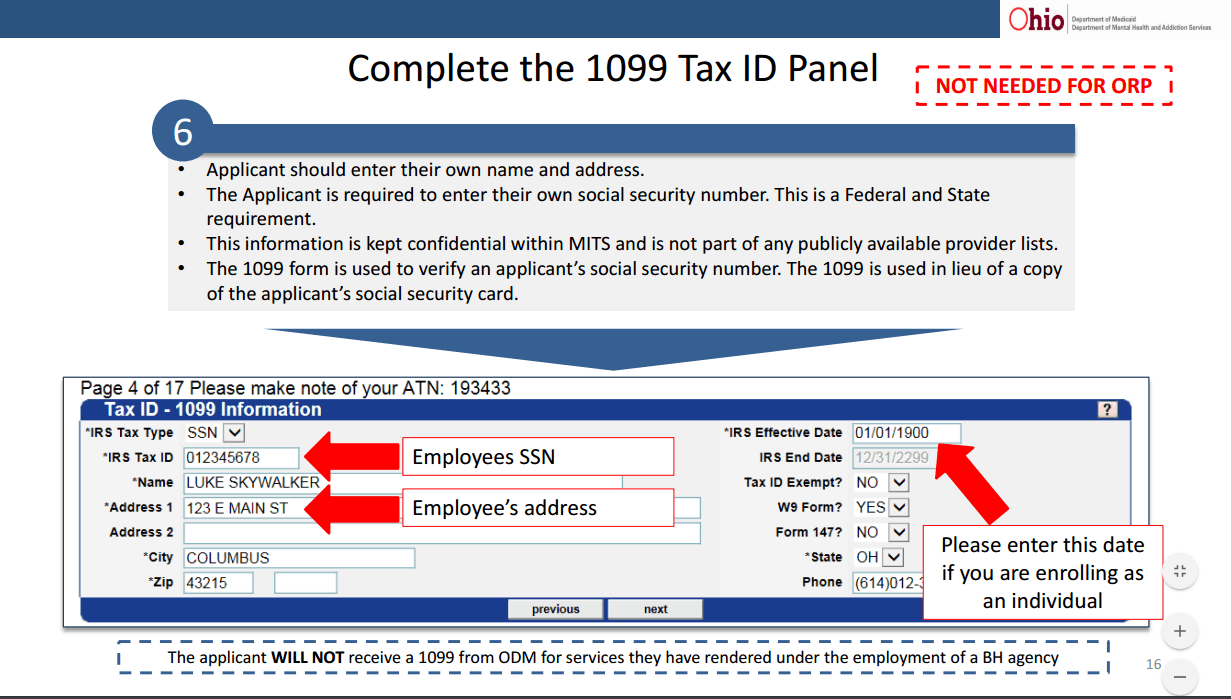
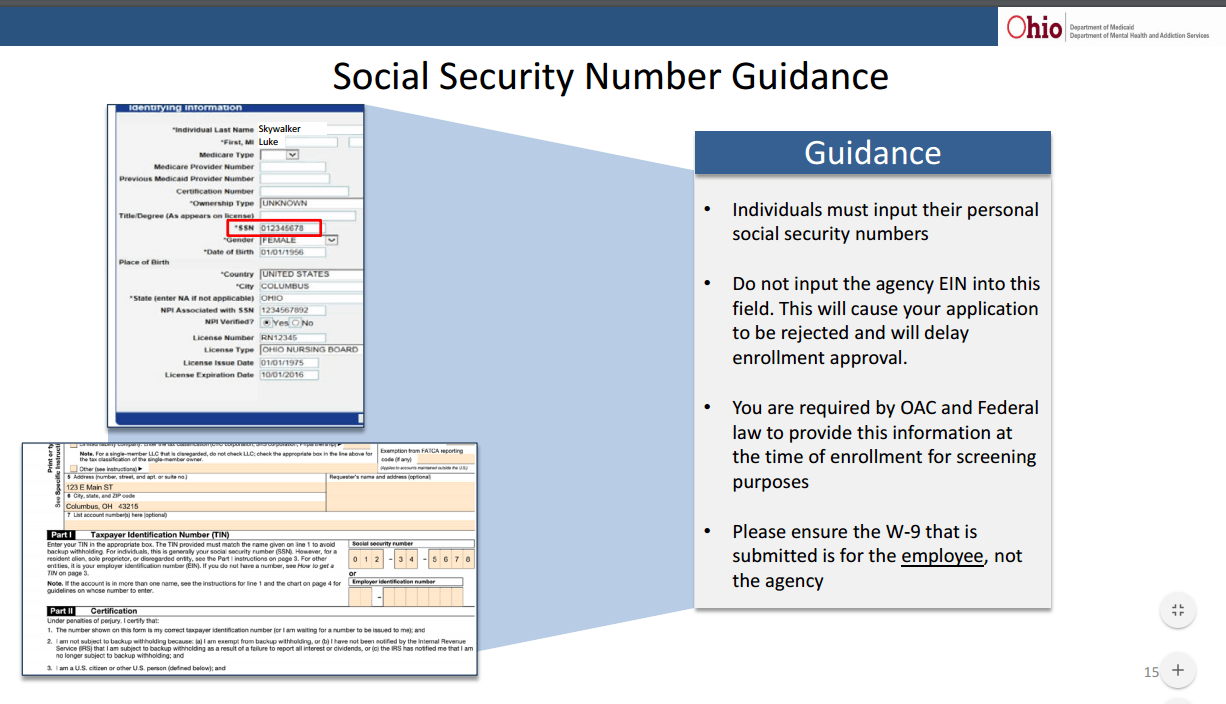
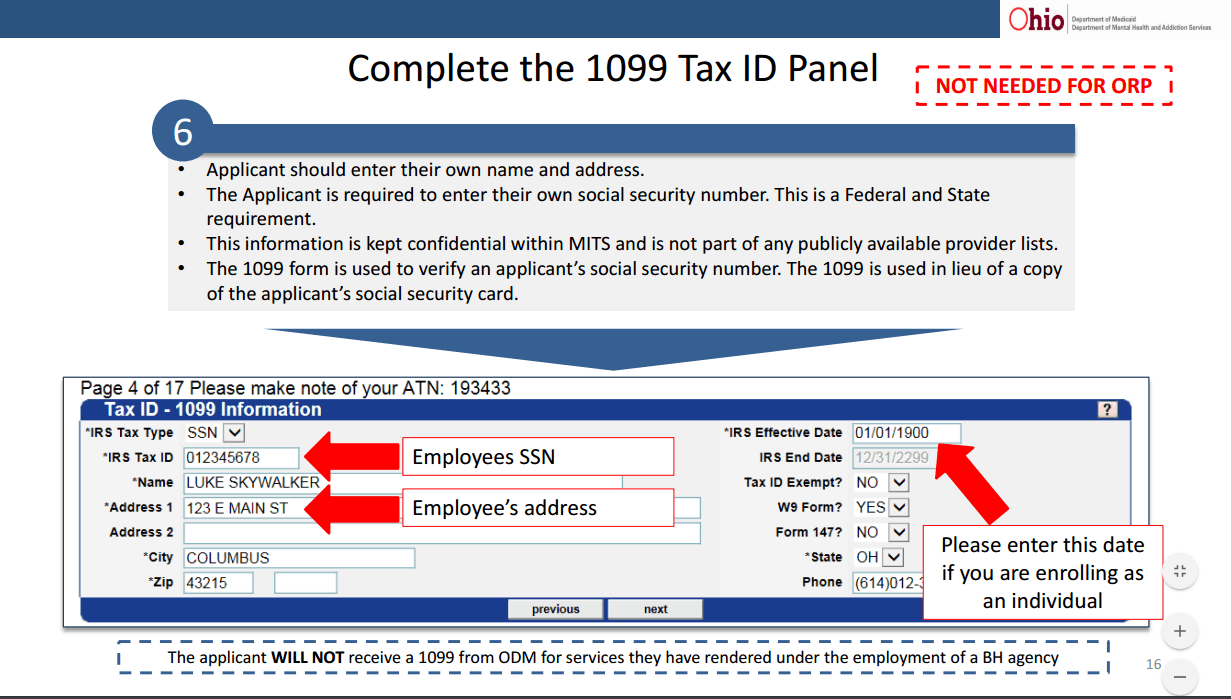
3. Still a lot of returned applications for registering providers, over 400 applications have been returned. Most likely cause is the required W-9. For individual providers registering with Medicaid for the FIRST time, the W-9 needs to be completed with your SS# and not your agency EIN. No, this does not mean you will in any way be charged for revenue your agency bills for, it just allows Medicaid to correctly search for additional detail on you to verify your credentials so you can be approved. A W-9 incorrectly completed will be returned. See below for information from the slides provided for step by step registration information.
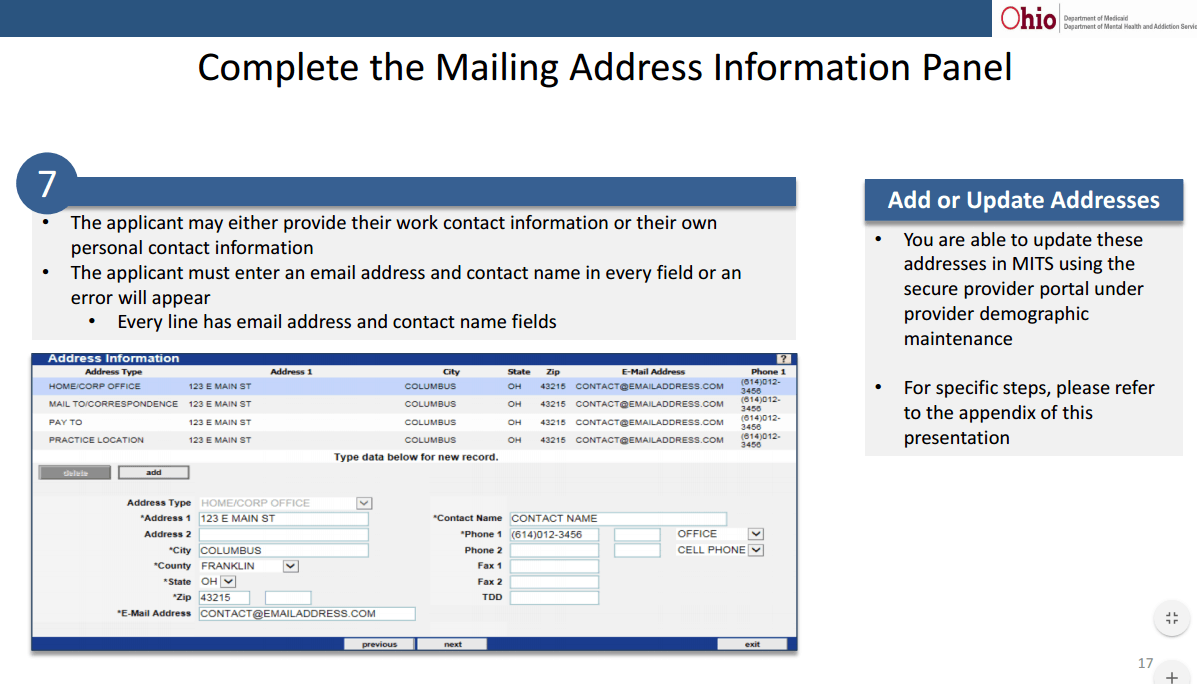
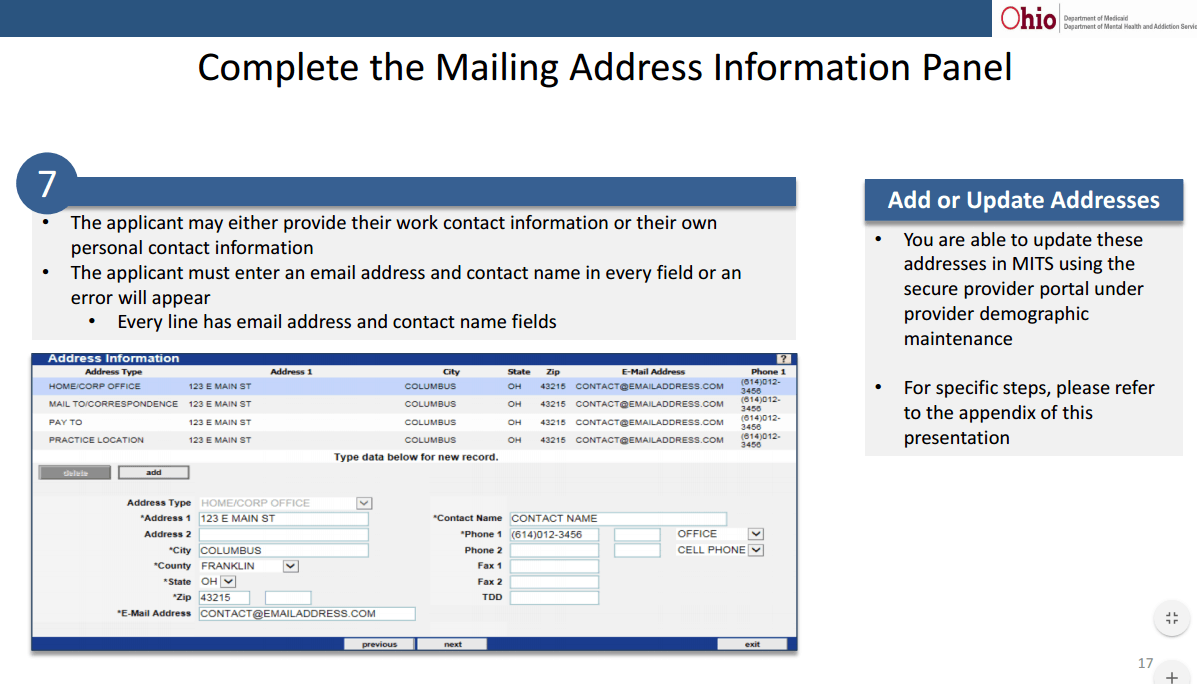
4. Another tip for registering providers. Whether your registration is completed by the provider or by a billing staff member on behalf of the provider, there is an important section needed to be completed so that any errors or final approval can be received by the provider and your billing staff who is tracking all registration. Be sure to add Practice Location, Pay to Location, and Mail to information using information related to your agency and not you as an individual provider unless you are truly a sole pratitioner. In anything practice related, enter your billing staff or administrator email and phone so they can receive any information related to incorrect submission or approval. This is a critical piece of missing information. According to Medicaid, as of yesterday, 285 applications have been returned to providers due to submission issues. Where did they go? To whoever is listed in the contact section pictured below.
Click the link to view the slide presentation pertaining to Provider Enrollment. If you would like assistance with any part of the registration process, please feel free to contact me directly through my Contact Us page on my website or by emailing directly to teresaheim@bhbillingsolutions.com.
Below is the link for the latest slide deck from the EDI Work Group.