Posted by Behavioral Health Billing Solutions, LLC.

Today I had the honor of providing testimony to the Senate Finance Committee on HB 49 in an effort to stress from a billing and information technology perspective why vendors and agencies will not be ready as of July 1st, 2017 and the potential impact to the communities we all serve.
I provided verbal as well as written testimony and I believe it was well received. It was fully covered by NBC 4 WCMH and video coverage of my testimony as well as an interview from Lori Criss from Ohio Council is covered in the story.
Select NBC 4 Mark Taylor to view
I would like to thank all of the Finance Committee Members for allowing me to speak with them today. They were attentive and seemed genuinely concerned about the information they were receiving. One piece of my statement I feel is something that I feel the need to highlight.
What does this mean to Ohio Behavioral Health agencies and the communities they serve?
It means that as of July 1st, a small percentage of agencies will be able to bill. The fact is, most agencies don’t have the level of
expertise to navigate the technical knowledge that is necessary to make this work if their software is not ready. So by August 31st, smaller behavioral health agencies in Ohio and perhaps larger ones, will be in financial trouble. When, not if, they dissolve, the impact to their communities will mean less access to service, longer wait times for treatment, and the public will not receive the treatment they need. This decreased access to service will inevitably lead to increases in crime, increased overdoses, and potentially an increase in alcohol and drug and mental health related deaths because people suffering with these diseases can’t get access to care. Not one of the systems I am testing from or have working knowledge of, have current functionality in place to meet the redesign needs today.
A decrease in access to service does nothing to assist with the epidemic in our state.
Let me close with the fact that I agree the proposed changes to behavioral health are needed for us to be compliant with national coding standards. And I must say the state departments involved have faced huge challenges in developing these changes and done an excellent job at listening to stakeholders and ensuring the changes do not negatively impact agencies. I’ve been very impressed with the entire team at the state level that I have worked with over the last year and a half as they build, develop, and provide training on these changes.
The fact is that once the Ohio rules that drive these changes are finalized, vendors and agencies should have 6 months to develop software, train billing staff and implement the necessary clinical changes at the agency level. As of today, those rules are not even final.
I appreciate the committee’s time today and reiterate my request to seriously consider HB 49 and the requested delay to the BH Redesign and Managed Care to January 1st, 2018 and July 1st, 2018 respectively.
A follow up to the EDI Workgroup on Wednesday, June 7th was requested today. The expectation is we receive the information we requested two weeks ago which includes:
How many Trading Partners have tested?
How many Medicaid providers they tested for?
What is the Pass/Fail Percentage on received files?
What is the reimbursement rate of Billed vs. Paid Claims?
In all honesty, we need these questions answered to ensure all vendors and agencies are ready as of July 1st, 2017.
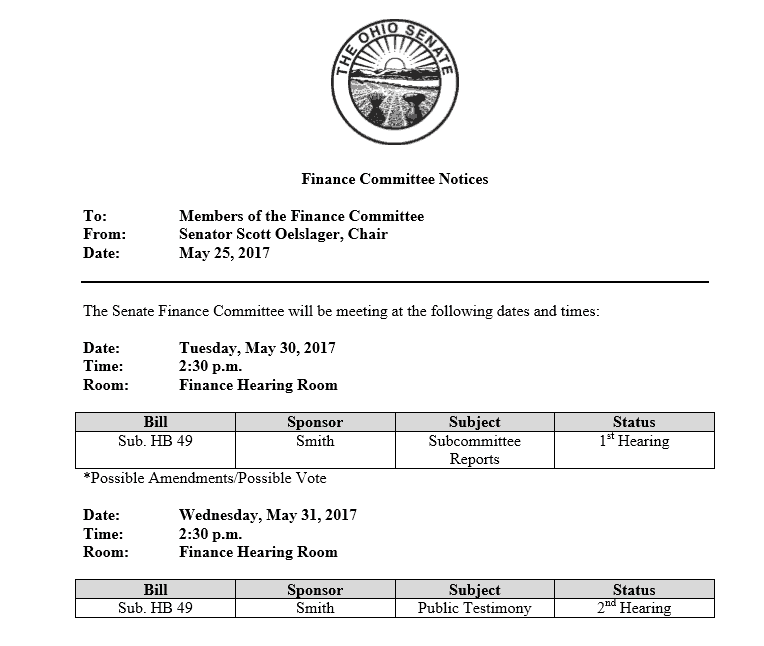
To view my full written testimony, please select the Finance Committee Notice below.

Thanks, great article.
Teresa, thanks so much for your continued hard work on this. As a small in-house EHR developer for our agency, having to make the July 1st deadline just for data entry (not billing!) would have been really, really tough… and even then it wouldn’t have been a finished product. A month or even more delay would be extremely helpful.
Hi Joe, I think I figured it out. I will send you something through Linkedin. I had an Ah ha moment when I read the latest development meeting slides.