Posted by Behavioral Health Billing Solutions, LLC
Dear Trading Partner,
It has come to our attention that some trading partners are not aware of the order in which EDI response transactions are returned after an EDI 837 Claims file submission. If you are not familiar with the process flow of files submitted to Ohio Medicaid, please see page 16 in the Trading Partner Information Guide.
If you have any questions please let us know. Thank you and have a great day!
My information posted in July 2017.
Medicaid changed the claims response process from a 277 to a 277U when it changed to OXI several months back.
Are you in the loop about the difference?
And how could this be impacting your agency?
Before I begin this post I want to state something important. If you are a Trading Partner for Ohio Medicaid, it’s critical that you have a process in place for reading all files related to your billing process. This includes your 837 billing file, 999 acceptance file, 277 claims response file and finally your 835 payment file. IF you are not, contact me directly as I can guarantee you are missing claim information that is critical to successful, complete billing and reimbursement. I use EMS Healthcare Informatics to read and interpret all the files I receive and recommend it for all my clients.
Below I will explain in more detail why this is important.
Several months back, Ohio Medicaid went to a new system for processing Trading Partner files. Prior to the change, the portal used to be a very easy to read and understand structure where all the different file types and error (trace) files were listed separately. Example below:
271 files (Eligibility Response)
999 file (Accept, Reject or Partial)
277 files (Claims Response)
835 file (Payment files)
Error (Trace directory)
In addition, we received a “True” 277 Claims response file which meant that every single claim included in a billing file was represented in the response file with a note of accepted or rejected and if rejected, a denial reason would be listed as a claim level or line level status description.
This also meant that all claims sent and received by Ohio Medicaid would have a response in your 835 payment file. The only time you would have a claim not returned is if in your 999 file, it indicated a rejected file or partial file acceptance.
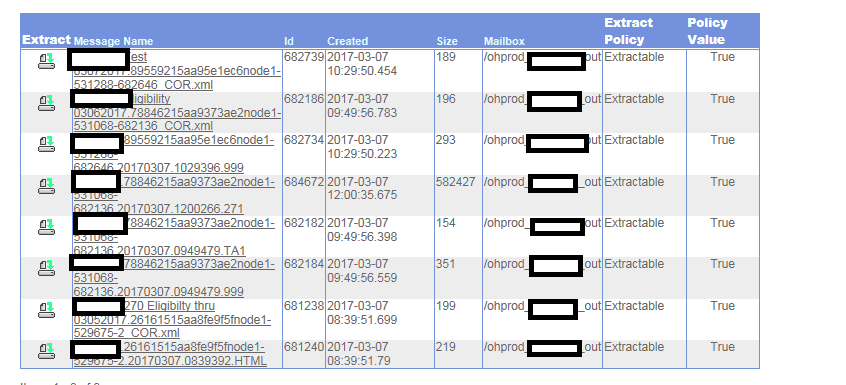
Early in 2017, Medicaid switched to OXI. Simply put, the response file structure is confusing to read, it’s difficult to find response files and even more difficult to read and understand. The files don’t even return in the same order they were sent. And the names returned automatically are 25 digits long and may or may not contain some of your file naming process in the response. Example below:
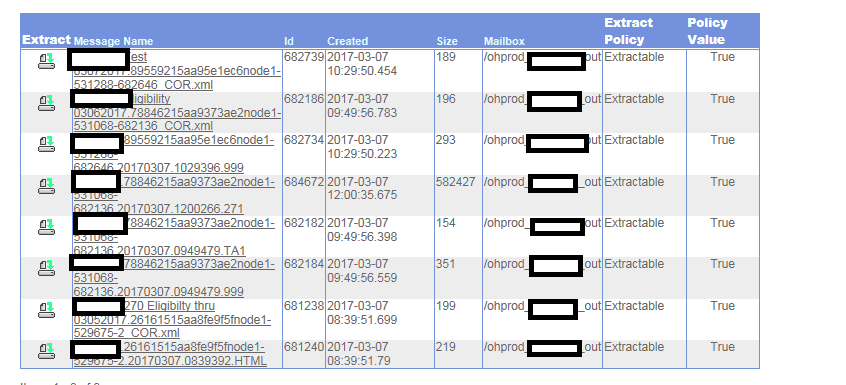
Even more important than our ability to read, extract and understand these files, is the fact that in March, they changed the way 277U’s adjudicate. Now they do not return every claim sent in all files. You may receive an 824 that lists incorrect Medicaid Id’s and a claim count of how many were thrown out of the billing file. This used to be indicated in the 277 as an 88 denial code at the claim level status under an A2 indicating the claim was accepted for adjudication.
What does this nonsense mean for you? Check the claim count of every 837 billing file sent since you switched to the new portal. Then check either the 277U or your 835 payment file against it and see if the claim count matches. If it doesn’t? You have a problem.
If you see variances, it means that although your system indicates a claim was billed, it never made it to Medicaid. It may or may not be included in an 824 file, it just did not make it through adjudication and therefore you will not receive a denial or a payment for the claim.
If you find an issue, my recommendation is first, contact EMS and get a reader. Then reach out to me if you need guidance on how to connect those exported files to find your missing claims. You can also open and attempt to read the 824 sent by Medicaid but I can’t say with certainty that it will contain information on all missing or drop claims.
The only other option is a full review of open billed claims with no response from Mediciad in your system.
 So today, Medicaid sent out the email below to Ohio Medicaid Trading Partner’s.
So today, Medicaid sent out the email below to Ohio Medicaid Trading Partner’s.