Posted by Behavioral Health Billing Solutions, LLC

The EDI work group met Wednesday, November 8th, 2017. Testing updates and changes to some coding was announced. Slides for the work group can be found here.
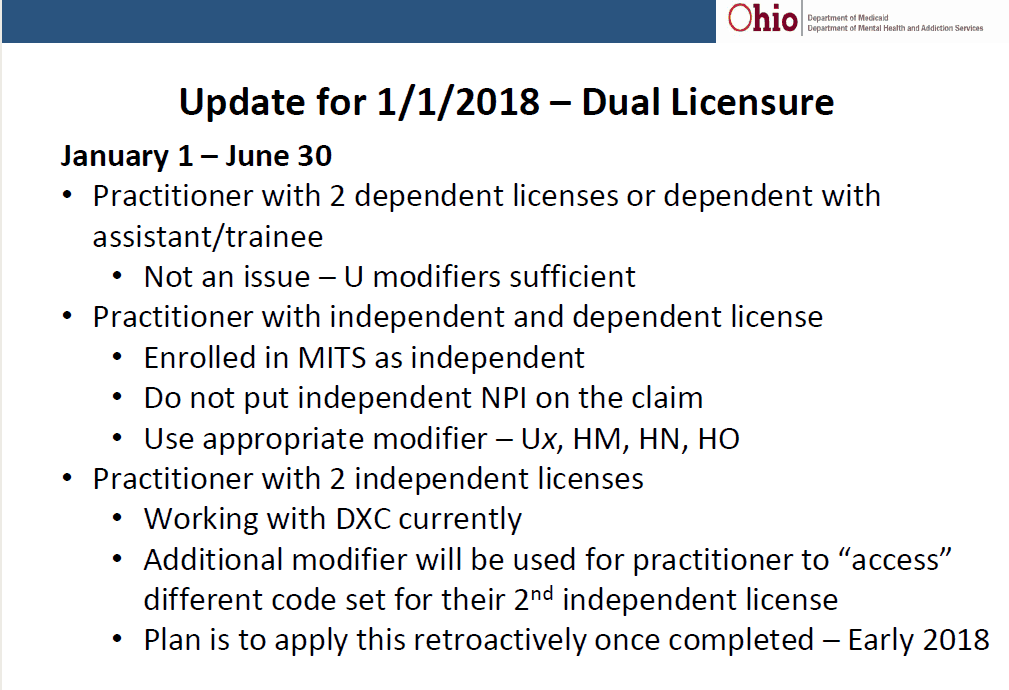
An important notification about the functionality of dual practitioners in effect retroactively in early 2018 was also announced.
In addition, a MITS Bits went out to all providers covering various testing info. To date, only 65 agencies out of approximately 650 have submitted test files. It is critical that ALL agencies across Ohio test their software programs and settings for Ohio Redesign readiness.

MITS Programming Errors That Are Being Corrected
As ODM has reviewed provider test claims, three issues have been identified and have been reported for correction. They are outlined below along with the expected date of their resolution in the test environment.
H0004 for SUD
• LSW, LMFT, LPC, LCDC II and LCDC III modifiers were not configured in the MITS test environment before testing began. This has been reported to DXC, the ODM vendor for the MITS system. Expected correction date is 11/15/2017.
H0004 for MH
• Code was not included originally in the test environment This code has been added to the test environment effective 11/3/2017.
Rate Correction
• H0015 UK is paying an incorrect rate for dependently licensed practitioners. This has been reported and it is expected to be corrected by 11/10/2017.
• H0015 TG, HK is paying an incorrect rate for dependently licensed practitioners. This has been reported and is expected to be corrected by 11/10/2017.
Changes Needed – In YOUR IT System for UT Modifier for Crisis Services.
Several managed care plans have reported their IT system cannot accept the UT modifier as it is no longer HIPAA‐compliant. The end result would have been denied claims for behavioral health services submitted using the UT modifier indicating service was rendered to a recipient in crisis.
To prevent this from this happening, the UT modifier must be replaced with the new modifier KX to indicate a service has been provided to a recipient in crisis.
Important change needed in your IT system: Your IT system needs to be updated to replace UT with KX for services rendered on or after January 1, 2018.
For testing, on 11/14/2017 the update will be made to the test environment to replace UT with KX modifier. This will affect test claims submitted 11/15/2017 and later.
Behavioral Health Redesign FFS Testing and Updates
BH Redesign Fee for Service (FFS) Testing ODM FFS testing has been underway for two weeks. To date, over 65 agencies have submitted test claims.
Based on ODM’s review of these claims, ODM has identified some common errors across providers that are causing some claims
to deny. Please keep these in mind as your agency submits test claims over the remaining three weeks.
Common Testing Errors
• Supervisor NPI:
Including for services or practitioners who do not require direct supervision
Supervising practitioner not valid supervisor for practitioner (ex: LISW cannot supervise a C‐T)
• Rendering:
No practitioner NPI or U modifier to indicate who rendered the service
Practitioner NPI and U modifier both reported
NPI of an unenrolled practitioner reported
NPI of a practitioner still pending enrollment
• RN and LPN Services:
RN or LPN reported as the ordering practitioner (RNs and LPNs must have an ordering practitioner but are not valid ordering practitioners)
RN code H2019 with LPN rendering
LPN code H2017 with RN rendering
• Modifiers:
Missing, incorrect modifiers (including use of existing modifiers instead of future modifiers)
• Procedure Codes:
Billing current code set instead of future code set
Billing decimal units (no decimal billing allowed as of 1/1/2018)
Billing add‐on code without the base code
Testing tips
Do not report supervisor NPI unless indicating direct supervision for CPT code
Test using the new codes under BH Redesign
Use rendering, supervising, and ordering practitioners who are currently enrolled in Medicaid.
Ensure enrolled practitioner is also affiliated with the billing agency
Always report either a rendering NPI or U modifier (not both)
Ensure recipient used on test claim is Medicaid eligible on the date of service
Avoid claims for recipients with third party insurance coverage