Posted by Behavioral Health Billing Solutions, LLC.

Rapid Response info, Prior Authorization training and the 1st week of BH Redesign – LIVE
The first week of BH Redesign Go live ended with a training on how to enter your claims on the MITS portal. Good training and they will be posting the video and once they do, I will share it.
The best question was “I’ve been entering claims on the portal all week and all seem to be denying or getting remarks. Did something change as of January 1st, 2018?”
I talk to agencies every day that were taken off guard by the changes. Many state their software isn’t ready, many don’t fully understand the rules that support these changes. And almost all, have a lack of full understanding about the complexity of these changes.
As an agency providing behavioral health in Ohio, you do have options. There is a contingency plan offered IF you do not feel you are ready and MITS portal claim entry is not an option.
&nsbp;
Realistically, if you have significant claim volume, it will be difficult to keep up and get the correct reimbursement through MITS portal claim entry. See below for information on how the contingency plan works.
| Jan. 5, 2018 |
| *** Contingency Plan for BH Providers – Advanced Payment Agreements
Ohio Medicaid has developed a contingency plan to assist community behavioral health provider agencies that need some extra time beyond Jan. 1, 2018, to update their electronic billing systems to submit EDI transactions and transition to the new coding requirements. NOTE: Providers may still use the MITS portal to submit Medicaid claims in lieu of EDI submission. This would alleviate the need to enter into a contingency agreement with ODM (see previous January 3rd MITS Bits on MITS Portal training occurring today for BH Providers). Providers that choose this option will be eligible for contingency payments under the following conditions:
Providers intending to utilize this option must return a signed copy of the BH Advanced Payment Agreement in PDF format to BH-Enroll@medicaid.ohio.gov by 5:00pm on Jan. 16, 2018. Providers can access the BH Advanced Payment Agreement HERE (it is also located on the BH website homepage). Below are important points to keep in mind when completing the BH Advanced Payment Agreement: If your agency is enrolled as both provider types 84 and 95, please sign and submit a separate agreement for each 84 and 95 line of business and include your corresponding 7-digit Medicaid billing ID. Each line of business will receive an advanced payment separately. Advanced payment agreements are intended only for behavioral health providers not ready to submit claims for dates of service beginning Jan. 1, 2018. Remember that the MITS portal is still open 24/7 for the submission of claims for behavioral health services rendered to Medicaid clients not enrolled with a MyCare Plan. These agreements are intended only for BH providers with a claims history in CY 2016. Advanced payment agreements will not be approved for providers new to Medicaid billing. ODM will inform the provider of their average monthly payment amount via email prior to first payment. ODM will make the monthly advanced payment for January and February together. The payments for March and April will be delivered in the early portions of each month. ODM will monitor BH claims submitted to MITS system for dates of service on or after Jan. 1, 2018. For claims submitted after Jan. 16, 2018, to MITS either electronically or via the MITS portal for dates of service on or after Jan. 1, 2018, ODM will terminate their advanced payment agreement.
|
BHBS does offer accurate MITS portal claim entry with a 100% guaranteed paid claim assurance on all fully documented services that are reimbursable. Contact us for more info.
&nsbp;
We also offer training on how to enter them yourselves as well as implementation support for your software. We know Ohio Behavioral Health billing and will work with you to get yours up and functional.
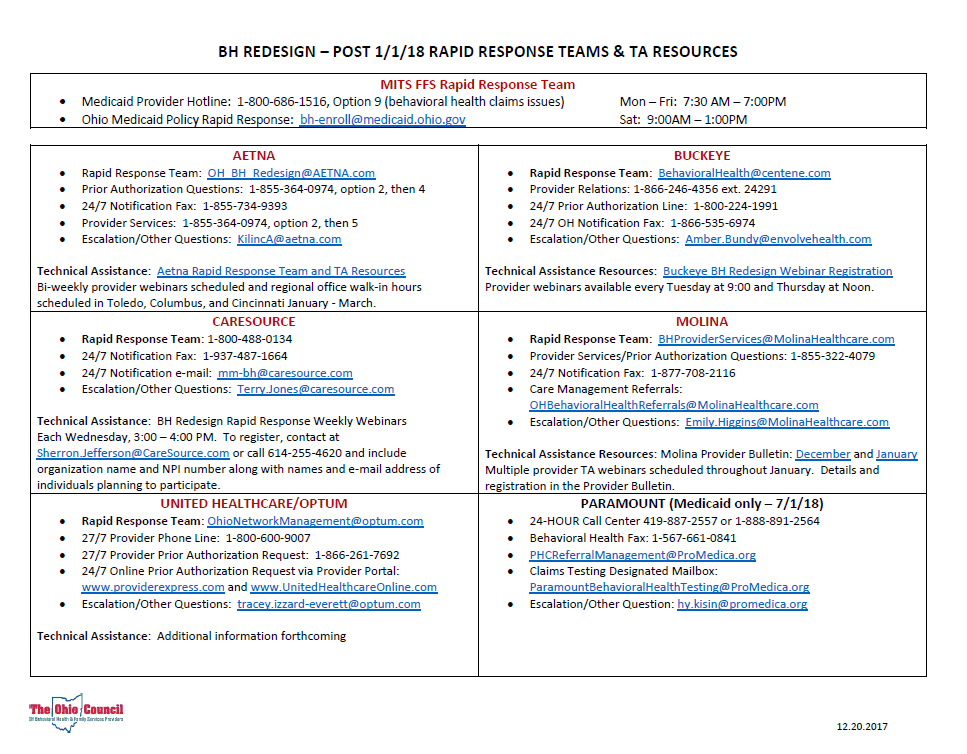
Last week, Ohio Council released a “Rapid Response” contact information sheet. Thanks, as always, to Council for this info.
&nsbp;
If your agency wants to stay in the know, become a member of Ohio Council. They support, advocate and literally stand up for their members when otherwise we may not be able to voice our concerns.
&nsbp;
We will be submitting our first EDI files this week, as will many agencies. As you prepare to do this, I have 3 important recommendations:
1. Check your client’s Medicaid eligibility PRIOR to submitting your first file.
2. Check your 277 Claims Response file. Review for any denials. Be sure to look at the claim level and line level denials. Together, they tell you how to understand the denial.
3. When your 835 comes back, compare it to your original billing file and 277 file. Ensure that you are FULLY paid for each service.
