Posted by Behavioral Health Billing Solutions, LLC.

How is Redesign going for your agency?
-
Are you submitting claims utilizing your software and submitting using an EDI file?
-
If you are, are you comfortable reviewing your 277 claims response file and 835 payment file to ensure you are getting paid correctly?
&nsbp;
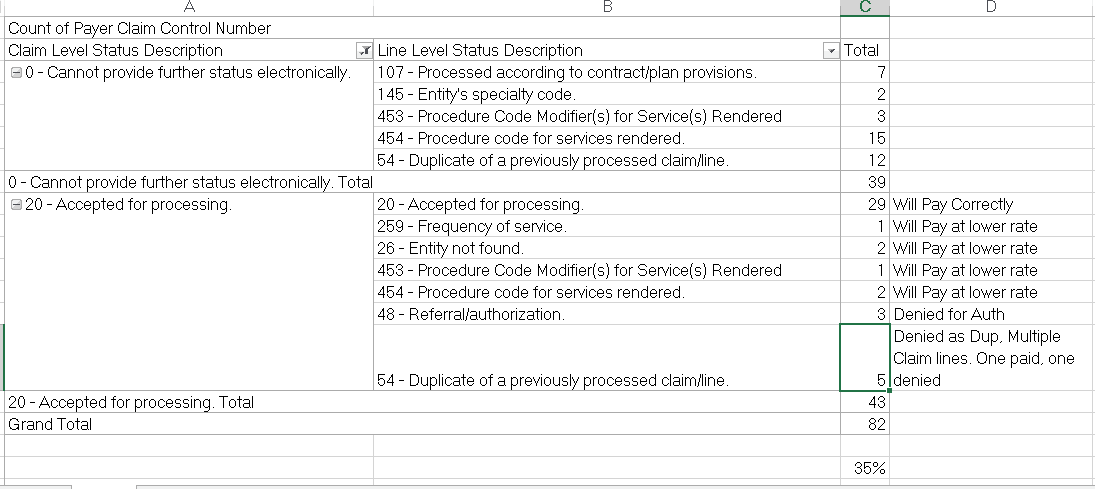
Below is an example of what a 277 claims response can tell you. This shows claims that were rejected, claims that were paid and furthermore, whether they will be paid at the billed rate.
&nsbp;
&nsbp;
This information is critical to understanding how your claims are paying and whether or not there is something you can do to rectify a denial on an accepted claim.
&nsbp;
For example, a duplicate denial on an accepted claim ALWAYS indicates that the claim contained more than one line. One paid and one denied. If both are valid charges, you can go into the paid claim and increase the units and dollars and resubmit and get paid for the full claim.
&nsbp;
My professional opinion is not all agencies will recognize these issues and understand how to correct.
&nsbp;
Net result? You don’t get paid the full amount for the service you provided, most likely because there is an error indicating the supervisor or licensure modifier required.
&nsbp;
In addition, I want to provide a quick reminder of a known issue.
&nsbp;
If you are submitting files through EDI submission, be aware that since March 2017, claims with an incorrect Medicaid # are thrown out of the billing file and placed in an “824” file. This file lists how many claims were impacted for each NPI and the incorrect Medicaid #’s. I’ve seen 824 files with hundred’s of claims thrown out that will never be properly adjudicated. It’s critical that each week you receive an 824, you read it, find the client with an incorrect Medicaid # and rebill all claims once it is corrected.
&nsbp;
Quick note: You can easily avoid these errors if you use Internet Explorer to search on the MITS portal and once found, double-click on the Medicaid # and copy and paste into your software. Also, check your eligibility using the EMS Power Generator, once a week to catch incorrect numbers.
-
Are you one of many agencies currently entering claims on the MITS portal?
-
Are you seeing denials and if so, do you know how to address?
-
How long does it take your staff to enter a claim?
-
Have you hit the daily maximum for data entry under your NPI?
-
Are you tracking the ICN and Paid amount for all entered claims?
&nsbp;
All of these questions or points, are important for you to be asking and monitoring for staff entering your claims.
&nsbp;
Every day you should know how many and what dollar amount were entered, how many denied and why, and what to do with the various scenario’s you will encounter.
&nsbp;
If your data entry staff is taking more than two minutes per claim and receiving denials for items other than eligibility, you need to look at the process being used. Unnecessary denials, slow data entry, incomplete tracking of claims, will all impact your bottom line.
&nsbp;
The first Medicaid EDI Work group was held the other day. Topics included known issues found during testing. timeline for registering dependents and unlicensed providers, and Medicaid’s solution for Dual Providers. And we should have a timeline for opening the registration of all providers shortly.
Slide deck is available here.
&nsbp;
