Posted by Behavioral Health Billing Solutions, LLC.

Change in Payment Cycle for Specific Fee for Service Providers
The Ohio Department of Medicaid (ODM) will be restructuring the timing of specific provider payment cycles beginning in April 2018. The Medicaid weekly payments scheduled for Thursday, April 5th will be delayed by one week permanently thereafter.
What this means is after this change your payment will no longer be for claims submitted the week prior. There will be a two-week delay.
For example, the expected provider weekly payment scheduled for April 5th, will be paid out on Thursday, April 12th.
The expected provider weekly payment scheduled for April 12th, will be paid out on Thursday, April 19th.
The expected provider weekly payment scheduled for April 19th, will be paid Thursday, April 26th.
The expected provider weekly payment scheduled for April 26th, will be paid Thursday, May 3rd.
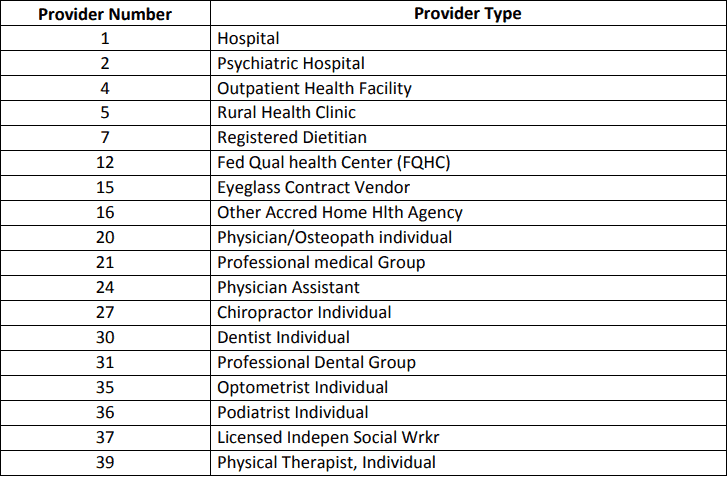
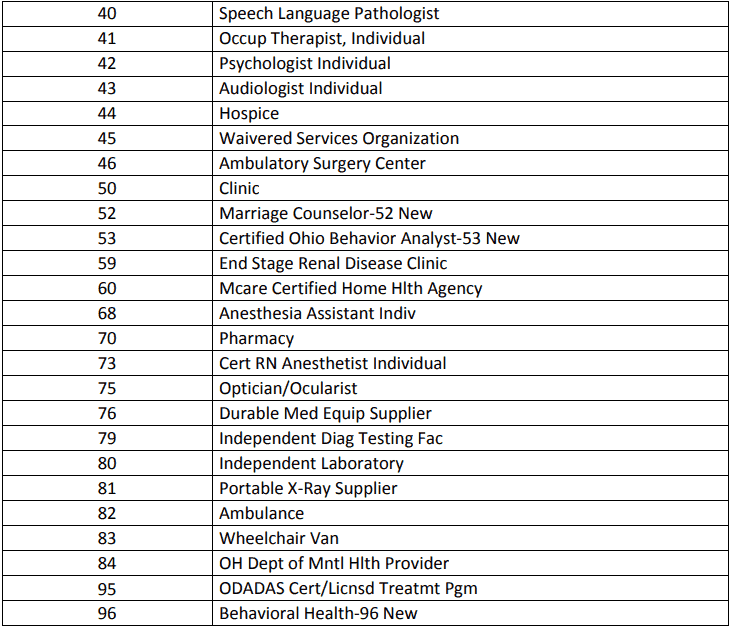
A complete list of provider types affected is available below.
&nsbp;
Please understand and prepare as this change will directly impact your cash flow during a time period that may already be challenged.
For complete information on these changes, please see the complete MITS release here.
As always, Behavioral Health Billing Solutions strives to be your resource for information, client or not. Feel free to contact us direct at 614-395-0136 or by email at teresaheim@bhbillingsolutions.com.
