Posted by Behavioral Health Billing Solutions, LLC

Ohio Behavioral Health Providers – Are you ready for the Managed Care carve in?
In January 2018, Ohio Behavioral Health Provider’s underwent a massive coding change. It’s referred to as the “Ohio BH Redesign”. Over the last 4 months several things have occurred.
-
Providers have struggled to get their systems to bill
-
Worked to ensure if they are billing, they are getting paid correctly
-
Found alternative methods for submitting claims, either through manual entry or creation of an 837 billing file without an EHR
-
Went through their lines of credit or eaten through any cash stores they have in order to keep the doors open
-
Struggled to report financial numbers for the first 3 months because of issues with understanding denials, what’s correctable that was denied, or even better did your files fail and you weren’t notified because they happened at the Tier 2 level
-
Attempted to adapt through a major payment change (one week to two weeks) that severely impacted many agency’s
Now we have less then two months to do the following:
-
Register ever single provider, (independent, unlicensed and dependent) with an NPI, CAQH and Ohio Medicaid. This includes registering a secondary credential for any provider that is dual licensed or licensed on one side and unlicensed on the other
-
Prep their EHR systems to deal with the changes in coding (which not all MCO’s are managing the same, see specs here). Keep in mind, we were under the impression all modifiers were going away and now we learn procedural and educational will still be in place AND we now have modifiers to use for dual providers. That info is available here.
-
Contract with the Managed Care company’s, which can take on average 90 days, start to finish and each are slightly different
-
Find a clearing house to send your Managed Care claims through, which in reality means you need some form of an EHR
-
Identify your client base’s MCO coverage, switch payers in your EHR or client record system AND keep in mind that CareSource and Paramount use a unique ID, other than your client’s Medicaid number.
-
Prepare financially for another major change in payment schedule. We are beginning to recover from a change of a one week payment schedule to two and now have to be ready to go to, at a minimum, a 30 day payment schedule. And don’t forget the fiscal year end, right before July 1st where Ohio BH providers will miss a payment
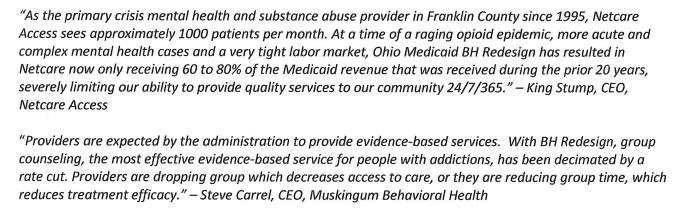
Recently, Ohio Council did a survey of their members to ask specific pertinent questions. Here is a link to the results of their survey. They also submitted the survey with this cover letter to the Joint Medicaid Oversight Committee which includes two quotes from providers that have been impacted by the Redesign.
In addition, Lori Criss, CEO for Ohio Council had an op-ed published in the Columbus Dispatch stressing the need for Ohio Medicaid to delay the managed care carve in. Available here.
In a recent article in the Akron Beacon Journal, they send a message to the Governor “to do no harm”. Specifically, The ABJ opines,
“…the purpose of the Behavioral Health Redesign is sound, and, surely, the many shortcomings that have
surfaced can be worked out. What the council survey shouts is: Make the corrections before taking the
leap into another new realm, managed care. For a state coping with a severe opioid crisis, the July 1 deadline is less important than getting the transition right.”