Posted by Behavioral Health Billing Solutions, LLC.

To address the looming deadline for the Managed Care Carve in, at Wednesday’s EDI meeting, ODM announced contingency funding available through the Managed Care Organization’s (MCO’s).
In addition to that, the MCO’s have submitted the letter below to Chairman Burke (JMOC) and Senator Terhar, committing to specific timelines for payment.
IS IT ENOUGH?
Read below and decide for your agency
May 29, 2018
Dear Chairman Burke and Senator Terhar,
The Medicaid managed care plans are committed to ensuring Medicaid members have access to needed behavioral health services and experience a seamless transition on July 1st when behavioral health services are integrated into managed care.
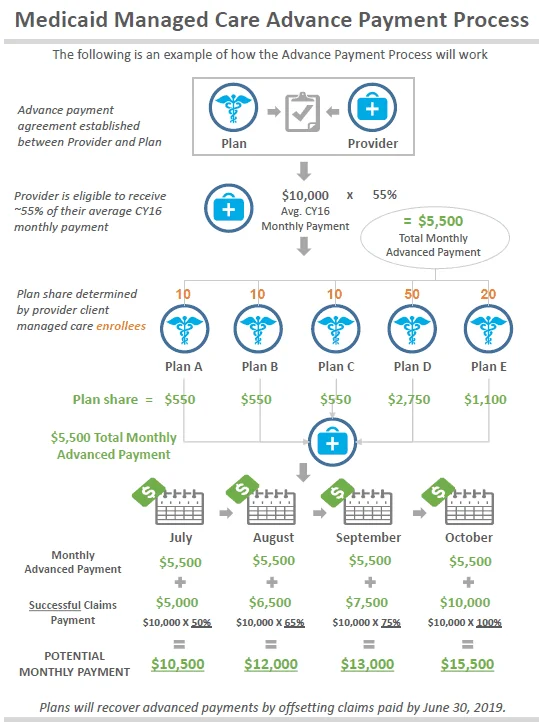
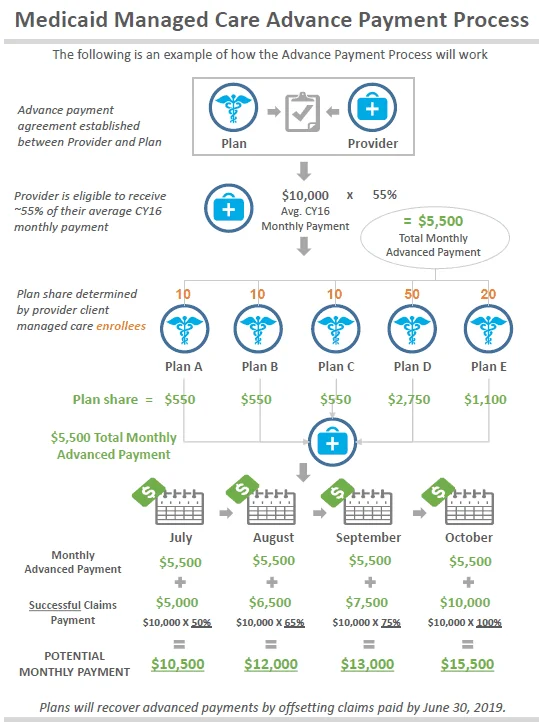
Over the past two years, we have been working tirelessly with ODM, OMHAS and behavioral health providers and stakeholders to ensure their readiness for both Behavioral Health Redesign and Behavioral Health Integration. ODM has conducted thorough onsite readiness reviews of all of the managed care plans ahead of July 1st and plans are on target for the July 1st integration. A number of member and provider safeguards are in place to ensure continued access to services including member transitions of care requirements through the end of 2018, maintenance of FFS coverage policies and rates until June 30, 2019, honoring prior authorizations approved under FFS until they expire, and a provider cash flow contingency payment plan.
You have asked the Medicaid managed care plans to provide a written commitment of a glidepath to further assist providers in the transition as it relates to timing of payments. The managed care plans agree to pay clean claims within the timeframes outlined below. Managed care plans will report this information weekly to ODM.
• For the month of July – pay 90% of clean behavioral health claims within 7 days
• August, September and October – pay 90% of clean behavioral health claims within 14 days
• November through December 31, 2018 – pay 90% of clean behavioral health claims within 21 days
• Beginning January 1, 2019 – pay 90% of clean behavioral health claims within 30 days per state law and Ohio Medicaid provider agreement.
We trust that the members of JMOC and the General Assembly keep the conversation open as we move through the implementation of integration to allow managed care plans the ability to share how this glidepath is working and the impact it is having on the program.
We stand ready to implement behavioral health integration in order to finally begin treating the whole person needs of our Medicaid members.
Sincerely,
Bruce Hill, CEO Steve Ringel, President Ami Cole, President
Buckeye Community Health Plan CareSource – Ohio Market Molina Healthcare of Ohio
Lori Johnston, President Tracy Davidson, CEO
Paramount Advantage UnitedHealthcare Community Plan of Ohio
We have some major concerns with the plans the MCO’s are recommending:
1. They don’t address the fact the provider enrollment of dependents and unlicensed provider’s are extremely lower than they should be. Current state, it would average between 8-10 providers per agency are enrolled and in most cases, 80% of an agency’s workforce are dependents and unlicensed.
2. CareSource has already stated that they are in the middle of IT and Staffing changes that are incomplete and they blamed these issues on causing the delay’s of payments experienced by providers in Qtr 3 and Qtr 4 of 2017. They should have to prove readiness to meet the timelines included in their proposals prior to this moving forward.
3. Agency’s are still struggling with billing post Redesign. We have absolutely no solid numbers to verify how many files failed, how many claims overall denied and an overall reimbursement percentage. The numbers Medicaid has provided do not tie to numbers BHBS is experiencing with a variety of clients so I believe an independent review of sent files and claims is the only way to actually gauge how Redesign is going.
4. We believe the communication between changes Medicaid is making and Managed Care plans needs substantial improvement. And not all plans will be managing claims in the same manner. These difference’s in claim submission are extremely problematic for software vendors.
5. Current state, many agency’s don’t have a mechanism or functionality available to them to generate and submit a 270 batch eligibility file to Medicaid or their clearing house to determine clients MCO affiliation OR the unique id’s used by CareSource, Paramount and United Healthcare. For more information on a tool that can generate a 270 file without an EHR, contact EMS Healthcare Informatics here.
6. What exactly is a “clean claim”? We believe we would like to hear a definition that explains exactly what that means. I believe it means properly adjudicated as sent. That does not mean paid, it means adjudicated.
If you have concerns about the impact of the Managed Care Carve in July 1st, reach out to your Senators and Representatives with specific’s as to why your agency would be negatively impacted.
House Representative Directory