 Posted by Behavioral Health Billing Solutions, LLC
Posted by Behavioral Health Billing Solutions, LLC
We hope all of you have survived “Snowpocalyspe” and are staying strong through the latest COVID surges. Behavioral Health Billing Solutions (BHBS), even though we are remote, has also felt the effects of COVID. It is an unfortunate reality that we are hoping and praying will pass sooner than later.
Professionally, and as it relates to our current and potential clients, it is an incredibly busy time. There is a lot to talk about.
MCO Procurement and PNM/Fiscal Administrator Timeline:
To stay in touch with ODM on the upcoming changes, visit Managed Care Reimagined
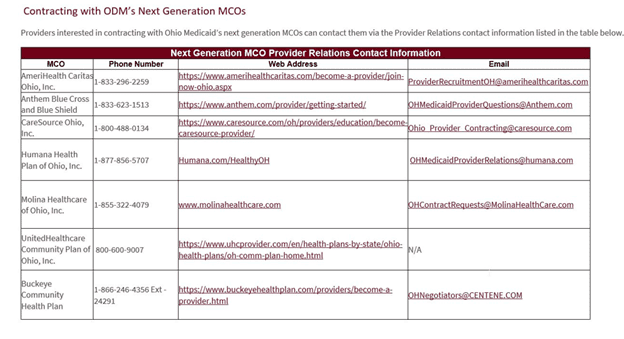
Centralized Credentialing, MCO Procurement, and the Fiscal Administrator are expected to go live on July 1st, 2022. Below is the contact information for the MCO’s. Ohio Department of Medicaid (ODM) is requesting that all agencies are contracted with the new MCO’s by February 1st, 2022 (already past), to be in the initial provider manual or listing on July 1st.
In addition to contracting with the new MCO’s and ensuring you are properly contracted with the current MCO, your independent providers will need to be registered and credentialed with CAQH. This is significant for behavioral health agencies that may be unfamiliar with the CAQH process since it was not “required” prior.
CAQH Registration
In addition, there will be new edits enabled that will reject claims if the provider is not correctly registered and affiliated to your agency MH and SUD NPI’s. A rejected claim will not be adjudicated by the payers, it is simply kicked out of the batch. At this time, we are unsure of how that data will be relayed back to Medicaid Trading Partners like BHBS. However, we are part of the Pilot Trading Partner group, so our hope is that we can assist with identifying problematic issues to make the transition smoother.
As for the Fiscal Administrator, this may cause some changes to your current workflow as an agency.
If you are sending your MCO batches directly through their portal and do not deal with a Trading Partner or clearinghouse, you will need to make some changes. Sending claims through the MCO’s portal will not be an option on July 1st.
If you are a ODM Trading Partner, all FFS, MCO, and Aetna Ohio Rise claims will go through the Fiscal Administrator (FI) and sent through your Trading Partner. MyCare, Medicare, Commercial, and Medicare Advantage will not go through the FI. You will need a clearing house to send those claims.
If you bill through a clearinghouse for all claims and are not a Trading Partner or have an affiliation with a Trading Partner, check with your clearing house for any potential changes and to be sure they are aware of the changes.
We would like to talk about the “MyCare plans won’t go through OMES statement above.” This is tricky to manage. MyCare plans initially came out for specific areas for Medicare/Medicaid clients. Since inception, they have transitioned the program, and there’s a mix of how you can see them, and they can be statewide. They could be traditional MyCare MDR/MCD; they could have Original Medicare and a MyCare MCD only plans. There are several ways they can be contracted. It will be essential for any agency billing directly through OMES that these clients are correctly identified and are billed through a clearinghouse, not the OMES portal.
All claims that will go through OMES, regardless of processor source, the client ID will be the ODM Medicaid number. Unique IDs will not be used. For Ohio Rise, we have yet to hear what ID will be used. In addition, we have been able to confirm that claim batches sent through OMES will need to be sent by Payer, not combined. Our opinion is that it will be an improvement we can build into our BHBS billing practices, but agencies trying to bill through their own Trading Partner need to be aware of this important change.
Because BHBS is an Active ODM Trading Partner, we will continue to offer our clients the ability to send their files through our TP and receive back your response files including 835’s, from FFS, the MCO’s, and Aetna Ohio Rise. And yes, this will decrease your current expense with the clearinghouse you utilize since ODM does not charge a per claim processing fee. However, you will still need a clearing house for Commercial, Medicare, Medicare Advantage and MyCare payers.
If we do not currently do this process for your agency, feel free to reach out, and we would be happy to discuss the process and explain the benefits of having us assist.
As stated earlier, Aetna Ohio Rise, the new statewide youth service program, will also go live on July 1st, 2022. The link to the website where information is available is Ohio Rise. BHBS will be testing for Aetna Ohio Rise through the ODM site as soon as all needed info is available. It will be built into our BHBS system and any stand-alone agencies that request the new fees and services on their own structure as soon as we get it. ODM completed an initial training on enrollment and the slides are available here at OhioRise Initial Training.
Additionally, we wanted to mention that we have recently added a line of service for Credentialing and Contracting, and we utilize the Intellisoft software to make the process more efficient. If you are interested in more information, please let us know. Our current client base will have the first availability to add this service, but we hope to assist new agencies as needed and grow internally to ensure the same quality of service continues. Current state, we know that on July 1st, we will shift to the new PNM. We believe use of the PNM will further improve this process because we will be able to see the beginning and end dates and affiliations better.
<31>HB 169:
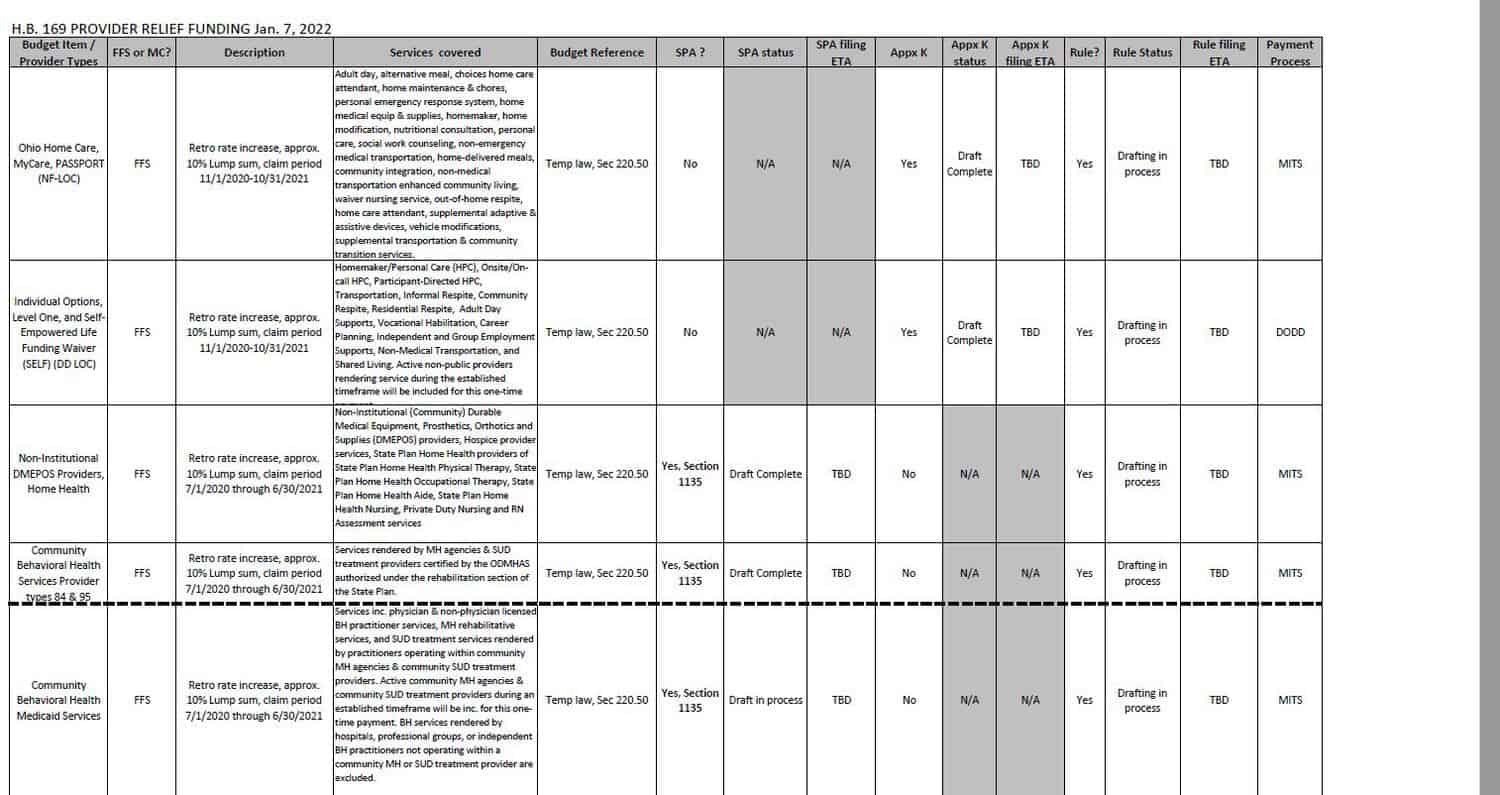
Another piece of recent good news is HB 169. We became aware of HB bill 169 the first week of January and are still gathering details. We have included the grid we received below. Community Behavioral Health Services, type 84 and 95 (our client base), will receive a lump sum retroactive payment for FFS and MCO paid claims for the time period of 07/01/2020-06/30/2021.
We are aware that even the most successful agencies are still feeling the impact of COVID, including reduced services, increased provider retention expenses, and much more. We are grateful that Governor DeWine and his team recognize that and continue to advocate for all Medicaid providers in the state. There is no firm date on the release of funds, but we got the impression that it should turn around relatively quickly, or at least that our my hope. Here is a link to the final analysis of the bill.
HB 169 Final Analysis Link
IHBT Enhancements Effective March 1st, 2022:
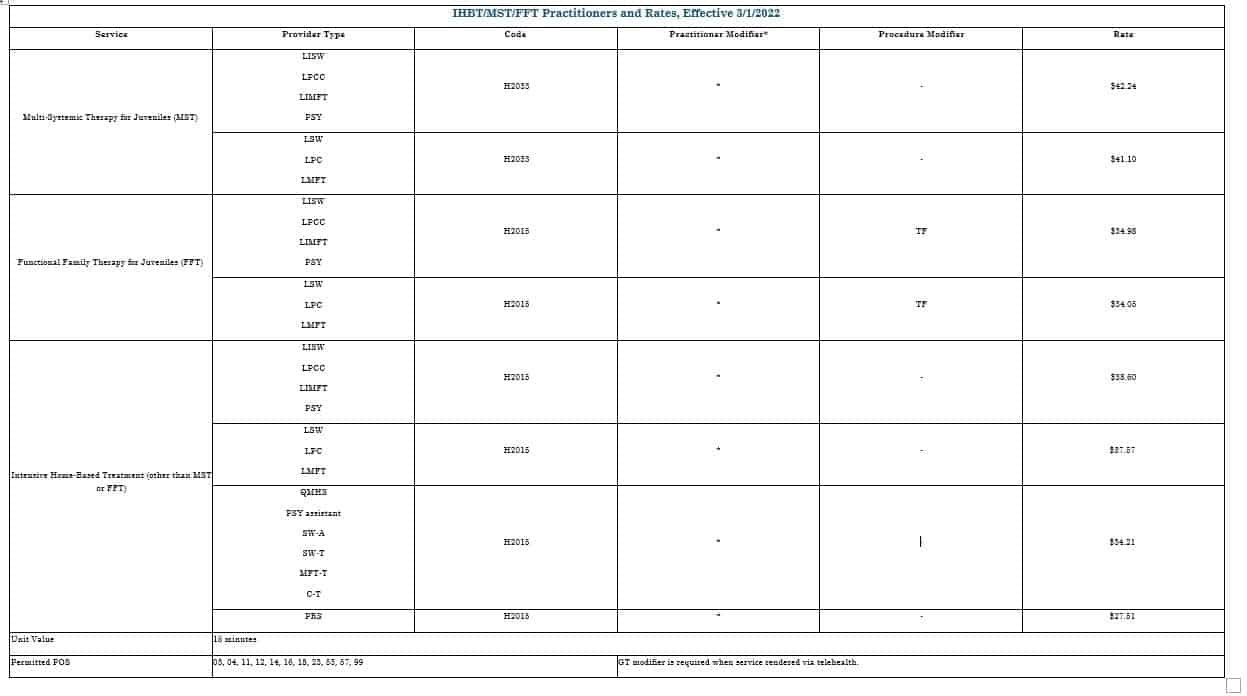
Effective March 1, 2022, the Ohio Department of Medicaid (ODM) and the Ohio Department of Mental Health and Addiction Services (OhioMHAS) will implement enhancements to the Intensive Home-Based Treatment (IHBT) service in accordance with new Ohio Administrative Code (OAC) rules 5122-29-28 and 5160-27-05. Medicaid billing and claims processing changes to be implemented for dates of service on and after March 1, 2022, include:
Updates to Medicaid payment rates, including new practitioner-specific rates.
The addition of qualified mental health specialists and peer supporters as eligible rendering providers of IHBT.
New billing codes and rates specific to Multi-Systemic Therapy (MST) and Functional Family Therapy (FFT).
Updates to diagnosis code requirements to include any valid ICD-10 diagnosis code for youth who meet the criteria described in new OAC rule 5122-29-28. (See “ICD-10 DX code groups” at Medicaid.Ohio.Gov under Provider > Manuals, Rates & Resources).
Changes have been made, as authorized in OAC rule 5160-27-05, to the list of behavioral health services that are allowed to be rendered to a youth receiving IHBT, MST, or FFT. (See the “ACT/IHBT” Excel spreadsheet at Medicaid.Ohio.Gov under Provider > Manuals, Rates & Resources).
IHBT services (including MST and FFT) will continue to be prior authorized and paid by the current Medicaid-managed care plans and ODM for fee-for-service members. Previous authorizations for IHBT will remain in effect.
ODM and the managed care plans will be ready to begin accepting and processing claims with these changes on March 1, 2022.
After the OhioRISE program is implemented July 1, 2022, IHBT services will be available only through the OhioRISE program.
ODM updated the Behavioral Health Provider Manual to incorporate these changes. Please see the detailed chart of practitioners, billing codes, and rates on Table 3-15 on page 77 and copied below.
ODM Managed Care Member Transition and Enrollment:
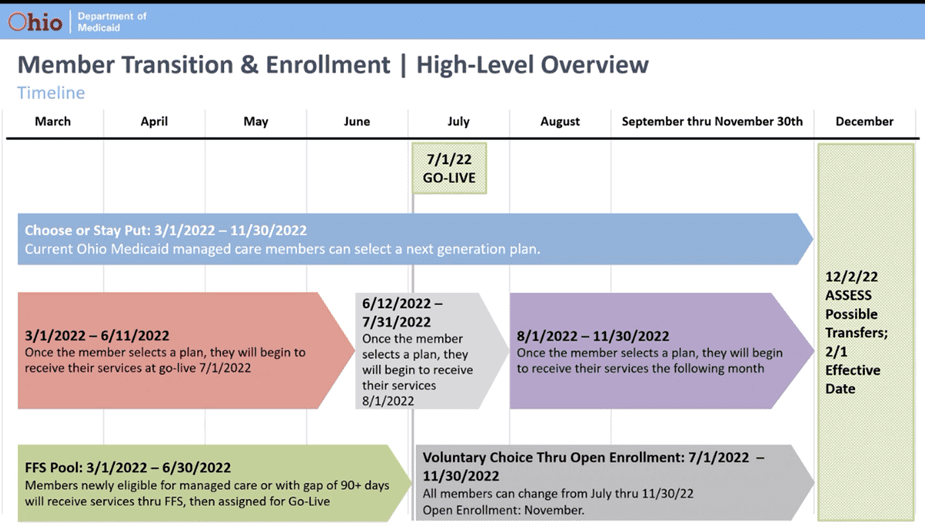
The Ohio Department of Medicaid hosted a series of listening sessions related to procurement implementation and provided updates on member transition enrollment. The transition enrollment to select from the seven new plans that will be effective on 7/1/22 is scheduled to open on 3/1/22. ODM’s transition enrollment encourages managed care members to actively select their MCO using a “choose or stay put approach” – but to affirmatively select a plan even if they want to stay with the plan they have. If a managed care member does not select a plan, then ODM will use an updated auto-assignment methodology to match the member to a plan that best meets their needs. For individuals with SPMI, OUD or a number of other chronic health conditions, the auto-assignment will default to the current Medicaid MCO. For those that do not have one of these conditions, ODM’s auto-assignment methodology will look at the individual/family’s current providers and make a match based on best fit. Individuals that were auto assigned into a plan will have the option of changing MCOs thorough 11/30/22.
Enrollment in the new Medicaid MCO will follow a rolling schedule. If a Medicaid member selects a plan between 3/1-6/11/22, that plan will be effective 7/1/22. If a Medicaid member selects a plan from 6/12-7/31/22 that plan will be effective 8/1/22. Additionally, Medicaid members will have an extended open enrollment and will have the option to change plans from 7/1/22-11/30/22. If a Medicaid member selects a new plan during this time, they will start on the new plan the following month.
FFS Medicaid Pool: Any new Medicaid member enrolling from 3/1-6/30/22 will be in Fee-for-Service Medicaid and then will be assigned to a managed care plan for 7/1/22. Providers may experience an increase in FFS billing to ODM from March-July of 2022.
In Closing:
In the coming months, we will be doing updates more frequently on our website. As always, we will post those updates to Linkedin and Facebook, so be sure to add us on both social media sites. It’s going to be critical that agencies are aware of the upcoming changes as they occur.
-
Facebook: Behavioral Health Billing Solutions Facebook Page
-
LinkedIn: Behavioral Health Billing Solutions LinkedIn page
We hope all of you and your families stay safe during this challenging time.
The team at Behavioral Health Billing Solutions
Contact us at ASK BHBS