Posted by Behavioral Health Billing Solutions, LLC.
So let’s take a minute to talk about the latest in update’s today in Behavioral Health in Ohio.
February has been a busy month in Ohio. The managed care companies have been doing “technical assistance” calls with agencies across Ohio. If you haven’t had yours, use the contact information here to find out who to reach out to.
They also had a mandate issued to pay for July services identified as outstanding in their systems on March 1st. Agencies had the ability to find out the amount in advance by emailing BH enrollment and asking. I haven’t seen anything about when August and September will be paid. It may be in a MITS BITS but like many agencies in Ohio, BHBS is no longer on the list to receive MITS BITS because the last two missed us.
How many of you didn’t receive these important notifications? Click here for the one that went out yesterday that I had to have Paramount forward to me as they explained that although an MCO asked me to have all of our clients fill out the universal roster, they cannot accept it because it’s not final yet. Hmmm, all of the other MCO’s have been working around that issue since I was unaware of it but it’s okay, I’ll spend Saturday night updating all of our clients to an “approved roster” for Paramount.
So basically, ODM and the MCO’s are going to a universal roster for providers and thankfully, agencies will have access to a list that shows HOW their providers are registered. See below for more details.
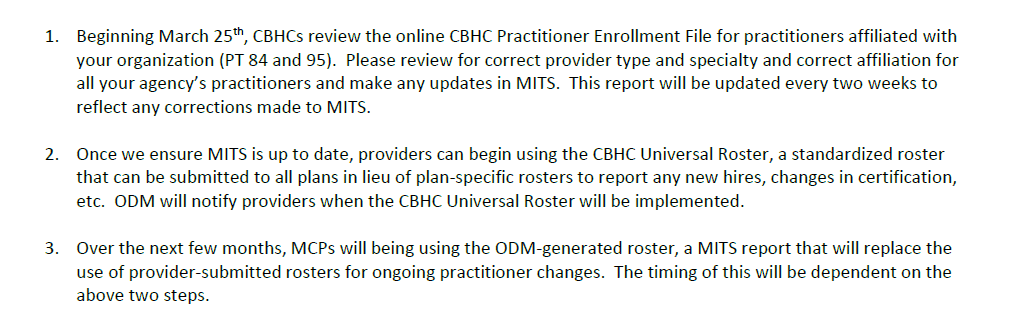
On March 20th, a training webinar will be held for CBHCs on the first step of the process, the CBHC Enrollment File.
Please enroll in the webinar here.
The webinar will share important information related to the use of this file which will be available online at: https://bh.medicaid.ohio.gov/manuals beginning March 25th. By the way, the manual was recently updated on February 22nd so I recommend everyone goes out and reviews it thoroughly for changes that have occurred.
There are still multiple adjudication errors occurring including short pays for direct supervision and licensure and a multitude of denials for prior authorizing for services that don’t require them. See here for a list of services that require prior authorization and the criteria surrounding them. I believe an MCO can decide to not require one on the list but I don’t believe they can require one for any not on the ODM list.
